
The plaque seen in Peyronie’s disease is benign, noncancerous, and not contagious or caused by any known transmittable disease.
The disease was named after the French surgeon François Gigot de la Peyronie who described it in 1743.
Usually men with Peyronie’s disease are referred to a urologist—a doctor who specializes in sexual and urinary problems.
Medical experts do not know the exact cause of Peyronie’s disease. Many believe that Peyronie’s disease may be the result of:
• acute injury to the penis,
• chronic, or repeated, injury to the penis,
• autoimmune disease—a disorder in which the body’s immune system attacks the body’s own cells and organs with low levels of the male hormone testosterone.
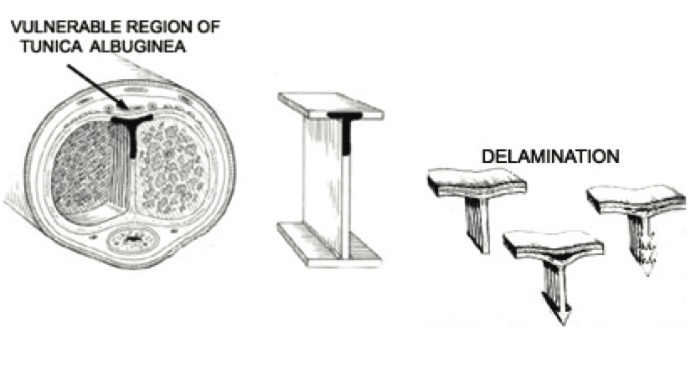
Medical experts believe that hitting or bending the penis may injure the tissues inside. A man may injure his penis during sex, athletic activity, or an accident. Injury ruptures blood vessels, which leads to bleeding and swelling inside the layers of the tunica albuginea.
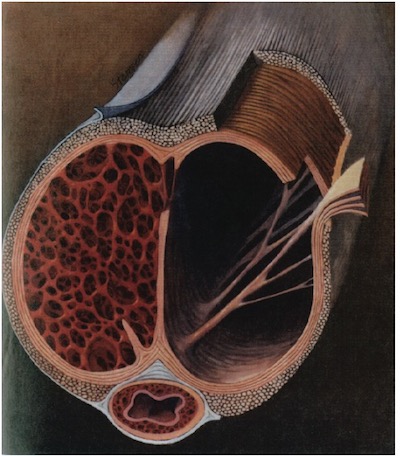
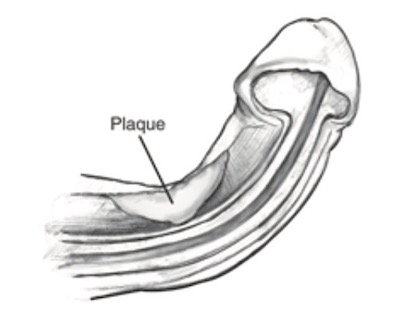
Swelling inside the penis will block blood flow through the layers of tissue inside the penis. When the blood can’t flow normally, clots can form and trap immune system cells. As the injury heals, the immune system cells may release substances that lead to the formation of too much scar tissue. The scar tissue builds up and forms a plaque inside the penis. The plaque reduces the elasticity of tissues and flexibility of the penis during erection, leading to curvature. The plaque may further harden because of calcification––the process in which calcium builds up in body tissue.
Some medical experts believe that Peyronie’s disease may be part of an autoimmune disease. Normally, the immune system is the body’s way of protecting itself from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances. Men who have autoimmune diseases may develop Peyronie’s disease when the immune system attacks cells in the penis. This can lead to inflammation in the penis and can cause scarring.
The actual occurrence of Peyronie’s disease may be higher due to men’s embarrassment and health care providers’ limited reporting. The disease is rare in young men, although it has been reported in men in their 30s. The chance of developing Peyronie’s disease increases with age. This condition is most commonly acquired at about age 55.
A man can be born with a curved penis, but this is not Peyronies disease but usually a penile curvature.
The following factors may increase a man’s chance of developing Peyronie’s disease:
• vigorous sexual or nonsexual activities that cause microscopic injury to the penis,
• certain connective tissue and autoimmune disorders,
• a family history of Peyronie’s disease,
• aging,
• connective tissue and autoimmune disorders.
Men who have certain connective tissue and autoimmune disorders may have a higher chance of developing Peyronie’s disease. A common example is a condition known as Dupuytren’s disease, an abnormal cordlike thickening across the palm of the hand. Dupuytren’s disease is also known as Dupuytren’s contracture. Although Dupuytren’s disease is fairly common in older men, only about 15 percent of men with Peyronie’s disease will also have Dupuytren’s disease. Other connective tissue disorders associated with Peyronie’s disease include:
• Plantar fasciitis - inflammation of the plantar fascia, thick tissue on the bottom of the foot that connects the heel bone to the toes and creates the arch of the foot.
• Scleroderma - abnormal growth of connective tissue, causing it to get thick and hard; scleroderma can cause swelling or pain in muscles and joints.
• systemic lupus erythematosus - inflammation and damage to various body tissues, including the joints, skin, kidneys, heart, lungs, blood vessels, and brain.
• Sjögren’s syndrome - inflammation and damage to the glands that make tears and saliva.
• Behcet’s syndrome - inflammation of the blood vessels
Medical experts believe that Peyronie’s disease may run in some families. For example, a man whose father or brother has Peyronie’s disease may have an increased chance of getting the disease.
The chance of getting Peyronie’s disease increases with age. Age-related changes in the elasticity of tissues in the penis may cause it to be more easily injured and develop the disease.
The signs and symptoms of Peyronie’s disease may include:
• hard lumps on one or more sides of the penis
• pain without erection or during sexual intercourse or during an erection
• a curve in the penis either with or without an erection
In addition to producing a curved penis, Peyronies disease may change the shape of the erection in other ways: indentation, diameter reduction, or loss of length.
Symptoms of Peyronie’s disease range from mild to severe. Symptoms may develop slowly or appear quickly. In many cases, the pain decreases over time, although the curve in the penis may remain. In milder cases, symptoms may go away without causing a permanent curve.
Complications of Peyronie’s disease may include:
• the inability to have sexual intercourse,
• Erectile Dysfunction (The cause for the erectile dysfunction of Peyronie’s disease could be a “venous leakage » , or psychogenic),
• Strong psychological impact – especially in single men and young men who are not in a well-established relationship, with a lack of self-esteem and a refusal for sexual intercourse.
Evolutivity of the painful period (not always) with erection usually lasts 6-8 months and is known as the inflammatory phase. This is followed by a fibrotic stage in which the pain settles but scarring continues to develop and the distortion of the penis continues. About half the men who get Peyronie's disease develop depression. Some cases are mild, healing without treatment within a year of onset. Most cases produce at least some degree of persistent curvature.
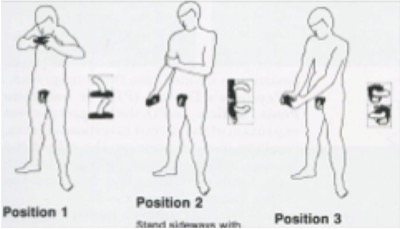
The typical symptoms of painful erections and curvature, angulation or deformity of the shaft are usually enough for a doctor to suspect that you have the disease. A urologist can usually feel the plaque in the penis with or without an erection to confirm the diagnose Peyronie’s disease. The deformation could be assessed by photographs taken at home
or after an intracavernous injection.
In most cases it is not necessary to do any other tests but, occasionally, you may be asked to undergo a type of scan called a duplex ultrasound which shows up the blood circulation of the penis after an intrac-cavernous injection and allows to take photgraphs. Sometimes, an MRI could be done to evaluatethe evolutivity, especially in young men and when the pain is durable.
One research study found that only 13 out of a 100 men got better without treatment. Of the rest, half had mild but continuing symptoms, the other half got increasing amounts of pain and/or curvature of the penis. With treatment, the situation can often be improved. However, more research is needed to investigate the effect of the various available treatments on prognosis.

A urologist may recommend surgery to remove plaque or help straighten the penis during an erection. Medical experts recommend surgery for long-term cases when:
• symptoms have not improved,
• the curve or bend in the penis does not allow the man to have sexual intercourse.
Some surgical methods can cause shortening of the penis. Medical experts suggest waiting 1 year or more from the onset of symptoms and 3 months witout any evolutivity before having surgery because the course of Peyronie’s disease is different in each man.
A urologist may recommend the following surgeries:
• Incision-Excision-Grafting: These procedures involve the replacement or expansion of scarred tunica albuginea with grafts of healthy tissue from another site. More recently, surgeons have been using grafts to expand the contracted scars (or plaque) without excising them. Though some calcified plaques still require removal, this non-excisional approach seems less disturbing to erectile function, and less likely to cause post-operative impotence. A urologist will cut or remove the plaque and attach a patch of a vein, or biomaterial. This procedure may straighten the penis and restore some lost length from Peyronie’s disease. However, some men may experience numbness of the
penis and erectile dysfunction after the procedure.
• Plications: This operation, or its various modifications, corrects bending by plicating the convex or outer side of the bend. Counteracting the relative shortage of tunica albuginea on the concave side straightens the penis, though length is reduced slightly as a consequence. Still, this procedure is less likely to cause numbness and erectile dysfunction than tissue grafting, and remains the first choice for moderate bends without associated diameter reduction.
• Penile implantation: A urologist implants a device into the penis that can cause an erection and help straighten it during an erection. Penile implants may be considered if a man has both Peyronie’s disease and erectile dysfunction. In some cases, an implant alone will straighten the penis adequately. If the implant alone does not straighten the penis, a urologist may combine implantation with one of the other two surgeries. Once a man has an implant, he must use the device to have an erection.

MHISC is a collective group of five International and European recognized surgeons. Leading experts from England, France, Italy and Serbia have been brought together to establish a global centre of excellence in the fields of genital and urethral reconstruction, erectile dysfunction (penile implants), peyronie’s disease, genital reconstruction for trauma, cancer and male infertility.
The idea is to create a base in Europe which will carry out the above surgeries and treatment in a bespoke, boutique private facility. Patients travelling to the centre would be offered the best treatment available in a comfortable and luxurious setting.
Given the nature of the procedures performed, confidentiality is paramount and therefore establishing a centre in Europe would allow patients from around the world to travel with discretion. This is particularly the case with patients from the Middle East who are currently travelling outside the Middle East to have their surgeries carried out by our specialists.
Ideally located between Geneva and Lausanne, Clinique de Genolier offers sweeping views of Lake Geneva, Mont-Blanc and the Alps. A presidential suite and junior suites furnished in contemporary style and “La Table”, a gourmet restaurant, ensure an exceptional standard of hospitality for the patients.
With 106 beds and 198 admitting physicians, it is one of the largest private clinics in Switzerland. Clinique de Genolier offers specialist medical care, one of the most up-to-date operating theaters in Europe, an experienced medical team and premier-quality hotel services.
To find out more about how we can help you please fill out the secure and confidential form on our contact page
Mens Health International Surgical Center SA,
Place des Philosophes 18, 1205 Geneva Switzerland